Lung Cancer Choices© 6th Edition Menu
Chapter 1: Diagnosis and Staging of Lung Cancer
Chapter 2: Comprehensive Biomarker Testing
Chapter 3: Surgery for Lung Cancer Patients
Chapter 5: Radiation Therapy for Non-Small Cell Lung Cancer
Chapter 6: Treatment for Small Cell Lung Cancer
Chapter 7: Clinical Trials and Emerging Therapies for Lung Cancer
Chapter 9: Nutrition in the Patient with Lung Cancer
Chapter 10: Sexuality and Lung Cancer
Chapter 11: Integrative Medicine, Complementary Therapies, and Chinese Medicine in Lung Cancer
Chapter 12: Lung Cancer in People who have Never Smoked
Chapter 13: How to Quit Smoking Confidently and Successfully
Lung Cancer Question Builder - Develop your list of "Questions to Ask" your providers
How to Quit Smoking Confidently and Successfully
Joelle Thirsk Fathi, DNP, RN, ARNP, CTTS, NCTTP
 Introduction
Introduction
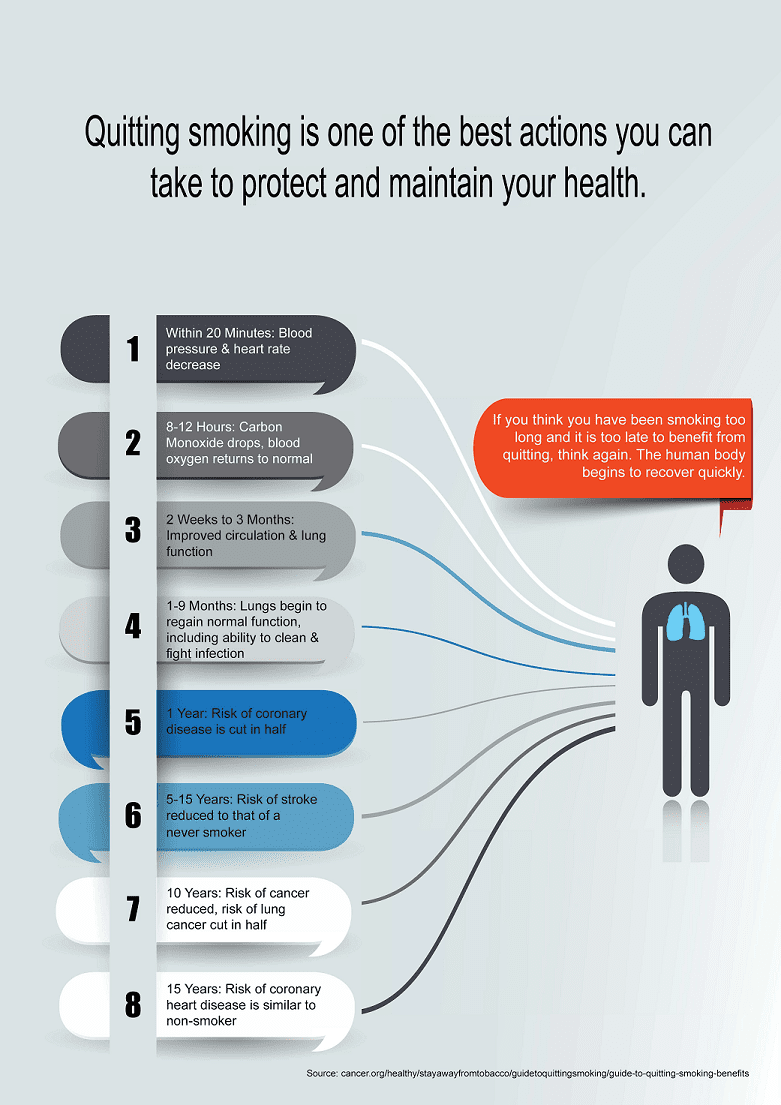
Smoking cessation (quitting smoking) is one of the best things to do to help our bodies protect us from disease, fight illness, undergo treatment, and help our bodies heal. Research shows that 70% of people who smoke want to quit, but only 7.5% are successful likely because they attempt to quit without help.1 There are many reasons people want to quit smoking, and better health is often at the top.2 Unfortunately, many people who actively smoke have had many unsuccessful quit attempts; this can be discouraging and prevent people from trying to quit again.
The chances of quitting smoking are 2-3 times greater with cessation treatment and therapeutic support.3 Knowing how to approach quitting smoking, find the necessary support, and be successful in quitting for good can be challenging. The content in this chapter provides the critical information needed to understand how nicotine dependence occurs, what happens when quitting nicotine, how to avoid the unpleasant symptoms of nicotine withdrawal, and most importantly, how to quit smoking safely and effectively.
Chemicals in Cigarettes
Cigarettes contain tobacco and up to 7,000 other ingredients, including many that are harmful to our health.4 When smoking a cigarette, toxic gases, including carbon monoxide (which is poisonous) and chemicals, such as tar, are inhaled and build up in the blood.5 These gases and chemicals circulate throughout the body and cause damage to the body’s cells. Additionally, cigarettes contain nicotine (the potent substance from the tobacco plant). Nicotine is the notable ingredient in all tobacco products, including cigarettes, that causes physical, mental, and behavioral dependence and makes it hard to quit smoking.6
How Nicotine Affects the Brain
When a cigarette is smoked, the combustible gases and chemicals are inhaled into the lungs and quickly travel from the lungs into the arterial blood and to the left side of the heart. The left side of the heart, with each beat, moves this oxygenated arterial blood, including the contents of the cigarette, out to the body’s tissues, organs, and straight to the brain. The transfer of nicotine, from the time a puff from a cigarette is inhaled to the time it is delivered to the brain, occurs quickly, within three to ten seconds.
How Nicotine Withdrawal Happens
Nicotine is clever in how it works in the brain; it easily attaches to receptors in the brain specifically responsive to nicotine, called the nicotinic acetylcholine receptors. Everyone has these receptors in the brain, but for smokers, these receptors are specifically stimulated by nicotine and respond in a way that the non-smoker does not experience. When the nicotine attaches to the receptor, the receptors are stimulated to release neurotransmitters (chemicals that your body makes) from that receptor. Dopamine is the most dominant neurotransmitter released when nicotine attaches to these nicotinic acetylcholine receptors, but other neurotransmitters are also released at this time. These neurotransmitters stimulate the reward center in the brain, creating a pleasurable experience that many people describe as a “brain buzz”. Dopamine and other neurotransmitters also enhance energy and concentration, elevate mood, and suppress appetite. The instant gratification and other physiologic responses to nicotine are all reasons why people continue to smoke, and dependence on cigarettes occurs and persists.6
The more cigarettes smoked, the more circulating nicotine is present and attaches to the nicotinic acetylcholine receptors. This results in higher dopamine levels in the brain. Nicotine is quickly metabolized, begins losing its stimulating effects soon after it is inhaled, and is gone within two hours. Once nicotine metabolizes and disappears in the body, tissues, and brain, the receptors are empty and stop expressing dopamine, and the dopamine levels drop. It is at this point that the receptors start begging for more nicotine, and withdrawal symptoms are experienced, which result in an increased urge to smoke.
Identifying Nicotine Withdrawal Symptoms
 The physical and mental changes that people experience when their nicotine levels drop can be difficult to cope with for many reasons. Most of the withdrawal experience is due to the drop in dopamine levels in the brain. Withdrawal symptoms can occur with any changes in nicotine use, including missing just one cigarette, cutting back on the typical intake of nicotine, or stopping the use of nicotine altogether. These symptoms, intensity, and frequency vary from person to person and directly correlate with the amount of nicotine that is routinely consumed and the concentration of nicotine levels in the body.5
The physical and mental changes that people experience when their nicotine levels drop can be difficult to cope with for many reasons. Most of the withdrawal experience is due to the drop in dopamine levels in the brain. Withdrawal symptoms can occur with any changes in nicotine use, including missing just one cigarette, cutting back on the typical intake of nicotine, or stopping the use of nicotine altogether. These symptoms, intensity, and frequency vary from person to person and directly correlate with the amount of nicotine that is routinely consumed and the concentration of nicotine levels in the body.5
Common symptoms of withdrawal include anxiety, irritability, agitation, and a drop in mood or even depression. People also experience disturbance in their sleep, difficulty with concentration, changes in bowel function, increased appetite, and urges to smoke.5 These symptoms are unpleasant and, for many intolerable. If not prevented or treated, these symptoms lead to a powerful urge to smoke again. Replenishing nicotine by having just one cigarette will ease or eliminate these symptoms. This is why people often revert to smoking because it makes withdrawal symptoms go away almost instantly.
When quitting smoking, staying away from cigarettes is the most crucial part of both short-term and long-term success in staying quit. There are proven methods of quitting smoking that minimize and even prevent the unpleasant and detrimental withdrawal symptoms from nicotine.
What it Takes to Quit Successfully
There are many ways to quit smoking and stay quit. People can quit on their own, but it can be a challenge to do this alone. There is a much higher chance of success when smokers can secure support and counsel from a health care professional or a specialist trained in quitting smoking. Using nicotine replacement therapy with or without prescription medication to quit at least doubles the chances of long-term success and, in some cases, even quadruples the chances of quitting for good.6-8
Options for Quitting Smoking: Nicotine and Non-Nicotine Therapy
Understanding the way nicotine affects the brain and how withdrawal occurs is important when quitting smoking. Moreover, knowing how to minimize and even prevent withdrawal symptoms is vital in successfully quitting. The following are descriptions of what is available to help people quit smoking and practical approaches to using these methods in quitting.9
Nicotine Replacement Therapy
Nicotine replacement therapy has been utilized for many years, is readily available, and can be a very effective approach to quitting smoking. Similar to the use of nicotine products, like cigarettes, the body absorbs the nicotine in the bloodstream and finds its way to the brain but the difference with nicotine replacement therapy is that toxic chemicals are not inhaled into the lungs. When nicotine from the replacement therapy reaches the brain, it attaches to the nicotinic acetylcholine receptors, which stimulates the release of dopamine and other neurotransmitters. Nicotine replacement therapy mimics nicotine delivery by a cigarette but delivers nicotine to the brain by another mode, thus preventing and treating withdrawal symptoms.6
 The most important thing to remember when using nicotine replacement therapy is to be sure to get enough nicotine replacement; if not used properly, it will not work to prevent withdrawal symptoms. Often people feel that the patch, gum, or lozenge did not work for them. This can occur because they were not getting enough replacement of nicotine to prevent symptoms of withdrawal. Getting enough nicotine with a combination of the long-acting patch and a short-acting method will prevent withdrawal symptoms, make quitting smoking much easier, and provide a smoother transition off cigarettes.
The most important thing to remember when using nicotine replacement therapy is to be sure to get enough nicotine replacement; if not used properly, it will not work to prevent withdrawal symptoms. Often people feel that the patch, gum, or lozenge did not work for them. This can occur because they were not getting enough replacement of nicotine to prevent symptoms of withdrawal. Getting enough nicotine with a combination of the long-acting patch and a short-acting method will prevent withdrawal symptoms, make quitting smoking much easier, and provide a smoother transition off cigarettes.
Transdermal Nicotine Patch, A Long-acting Nicotine Replacement
Nicotine replacement is available in a patch that delivers nicotine continuously over 24 hours.8 The patch is a long-acting delivery method that delivers a steady amount of nicotine to pass, from the patch, through the skin, directly to the blood with immediate transport to the brain. It is important to dose the patch according to how many cigarettes are smoked in a day so that enough nicotine is available to prevent withdrawal symptoms. One cigarette contains about 1mg of nicotine. The patch should be dosed 1mg for every cigarette smoked in a typical day. Choosing the right dosed patch will give an optimal nicotine delivery to the brain and minimize or prevent withdrawal symptoms.7, 9-10
Patch Dosing Recommendation9
| less than10 cigarettes/day (less than a ½ pack per day) | 14 mg patch |
| 10 or more cigarettes/day (1/2 pack per day or more) | 21 mg patch |
| more than 20 cigarettes/day | Dose patch to the number of cigarettes smoked per day with the guidance of your health care provider |
The patch needs to be changed every 24 hours. It is recommended to use the initial patch dose for one entire month and then step down the patch doses every 2-4 weeks until off the lowest dose.
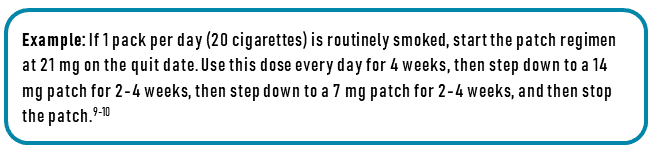
In this example, the nicotine replacement patch would be used for a total of 8-12 weeks (2-3 months) following the quit date; this ensures a safe and effective transition off nicotine. This is longer than many people think they need to use patches. Remember, the key is to be successful in the long run so, wean off as slowly as needed; there is no rush!
The patch delivers relatively steady levels of nicotine, but breakthrough urges to smoke can occur. This is where short-acting nicotine replacement therapy can be beneficial in further shutting down the cravings to smoke.
Short-acting Nicotine Replacement
Nicotine replacement is available in several forms of short-acting delivery methods. These short-acting doses of nicotine are essential in the success of using nicotine replacement therapy in quitting smoking. Even if the transdermal patch is used continuously for nicotine replacement, break-through urges to smoke could occur and lead to withdrawal symptoms. Think of short-acting nicotine replacement as a quick-acting, rescue medication. Treating these cravings with one of the following four options of nicotine replacement in combination with the long-acting patch is one of the most effective ways to avoid lapsing or relapsing with a cigarette and returning to regular smoking patterns.
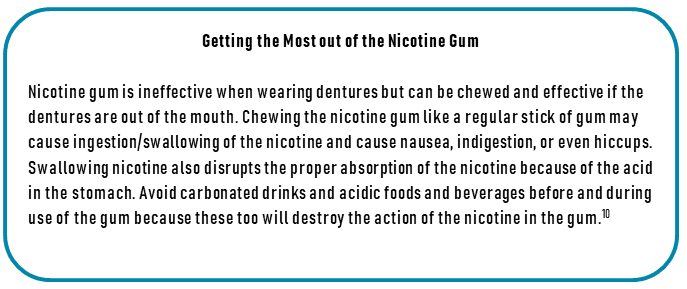
Nicotine Gum
Nicotine gum is available in 2 and 4 mg doses. It is important to know that the gum only works if it is absorbed through the mucosal lining of the mouth (between the gum and cheek). The best way to use the gum is to start with the lower dose first, chew it until there is a peppery/spicy, tingly sensation, then park it between the gum and cheek for 5 minutes. Then chew it again until there is another sensation (about a minute) and park it. Continue this pattern for about five cycles (approximately 30 minutes total) to get the full dose of nicotine the gum has to offer. Chewing for a minute is necessary to activate and release more nicotine in the gum, then park it for optimal absorption. It is safe to chew up to 20 pieces of gum a day for breakthrough cravings and withdrawal symptoms.7, 9-10 This product is available over the counter for purchase. Many insurance companies are now covering this when prescribed by a health care provider.
Nicotine Lozenge
The nicotine lozenge is similar to the gum. It is available in 2 and 4 mg doses and, like the gum, needs to be parked between the gum and cheek to be optimally absorbed. The standard starting dose is the 2 mg lozenge, which delivers the equivalent of nicotine in one cigarette. Like the gum, avoid eating and drinking acidic foods and beverages right before and while a lozenge is in the mouth. This product is also available over the counter and by prescription.7, 9-10 These lozenges vary in size and dissolvability by the manufacturer. Although some are cheaper over the counter, these products are often reported by people to be too big and bulky and take too long to dissolve in the mouth. There is a “mini” lozenge on the market that is the size of a Tic-Tac, is easily tucked between the gum and cheek, and dissolves readily while delivering nicotine quicker to the brain.
Nicotine Nasal Spray
Nicotine nasal spray contains nicotine that has the quickest onset of action in treating nicotine cravings and is delivered through the mucosal wall of the nose. When instilling this nicotine, it is important to spray it against the nasal wall while plugging one nostril (side of the nose) and (while looking at the floor) inhale while spraying. Avoid tipping the head back and sniffing it into the upper region of the nasal passages or sinuses. One spray in each nostril delivers a similar dose of one cigarette (two sprays total). This product is available by prescription only7, 9-10
Nicotine Inhaler
The nicotine inhaler is a popular method of short-acting nicotine delivery for people who have a strong attachment to the ritual of holding and handling a cigarette, but many people and health care providers do not know about it. Although this is called an “inhaler”, the nicotine delivery is taken in by puffing on the inhaler, not taking a deep inhalation, or “drag”, as would be done with a cigarette. The nicotine is absorbed through the mucosa of the mouth, so it is important to only puff it into the mouth (as if you are sucking on a straw) for optimal absorption. This product is available by prescription only7, 9-10 which is different from an E-cigarette, which is discussed later in this chapter. A dispensing pharmacist can teach how to load and use the inhaler. The inhaler is not effective if dentures are in place.
How to Know if you are Getting too Much Nicotine Replacement
It is possible to use/take in more nicotine in the nicotine replacement than you are accustomed to when regularly smoking or using other tobacco products. Symptoms associated with getting too much nicotine are feeling anxious, jittery, headache, nausea, excessive wakefulness, and chest pain or heart palpitations. If you develop these symptoms or any others that you think are associated with nicotine delivery, stop using all nicotine products, including taking the patch off, and call your health care provider for further advice as soon as possible. Remember to avoid smoking cigarettes or using other manufactured tobacco products (chewing tobacco, snus, snuff, electronic cigarette, etc.) while using any nicotine replacement therapy to reduce the chances of overdosing on nicotine. This will provide the best opportunity for you to quit.
Non-Nicotine/Prescription Medication Therapy Options
Bupropion Sustained Release
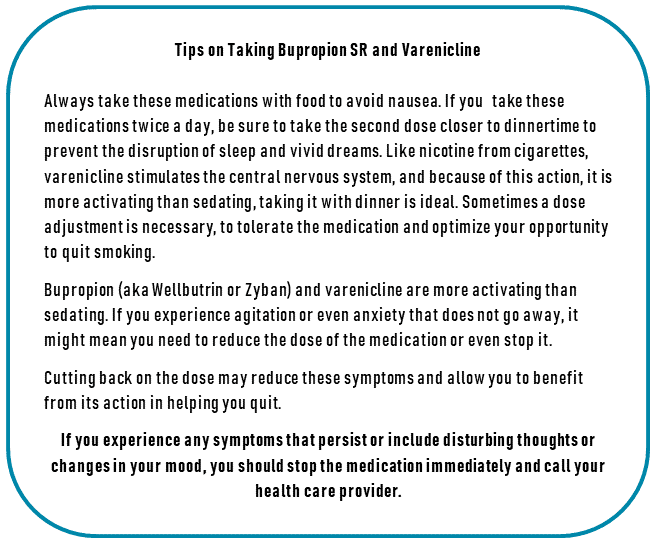
Bupropion Sustained Release (SR) is a long-acting prescription medication commonly used to help people quit smoking. It has been shown to increase the chance of quitting smoking by 52% to 77% and is as effective as nicotine replacement therapy.11 Bupropion SR may also be combined and works well with the nicotine replacement therapies. It is also known as “Zyban” and “Wellbutrin”.
Some people are hesitant to take this medication because they have heard that it is used for depression and do not want to take an “antidepressant”. This is true; bupropion is used for depression because it allows more neurotransmitters, like dopamine and norepinephrine to circulate in the brain.
Remember that nicotine drives the dopamine levels up, which is why the brain experiences a mood elevation when smoking. When the dopamine levels drop with nicotine withdrawal, the brain can experience agitation, anxiety, and depressive mood changes. Bupropion helps transition off cigarettes/nicotine because it allows more dopamine to circulate and prevents the brain from experiencing an abrupt withdrawal of dopamine. It reduces the craving for cigarettes, helps with the anxiety of quitting smoking, and often suppresses appetite, and controls weight gain associated with quitting smoking.5-7, 10 Talk to your health care provider to determine if bupropion is the right medication for you.
Varenicline
Varenicline (also known as “Chantix”) is a prescription medication commonly used to help people quit smoking. Varenicline has shown an increased success rate in quitting smoking of up to fourfold10 and is more effective than bupropion11 and nicotine replacement therapy.12
This medication works by attaching to the same receptors in the brain and causes the same release of dopamine that nicotine does. Varenicline mimics the presence and action of nicotine and tricks the brain into thinking it has nicotine onboard.5-7, 10 Because of the way this medication mimics the presence of nicotine and attaches to the nicotinic acetylcholine receptors in the brain, it is not designed to be used in combination with nicotine replacement therapy unless directed otherwise by a health care provider.
This medication greatly reduces the craving for nicotine and reduces withdrawal symptoms. Talk to your health care provider to determine if varenicline is the right medication for you.
Vaping/Electronic Nicotine Delivery Systems (e-Cigarettes)
Many people are asking about the use of electronic cigarettes, also known as e-cigarettes or “vapes”, as a replacement for conventional cigarettes or as aids in quitting smoking. Vaping and electronic cigarettes are battery-operated devices that deliver nicotine and other chemicals to the body through an inhaled vapor or aerosol rather than a combustible gas, as cigarettes do. Some people feel that vapes and electronic cigarettes may be safer for their health because they do not “light up” or create combustible gases while using them. Recent research demonstrates a higher quit rate for people who use electronic cigarettes with nicotine than people who use electronic cigarettes without nicotine.13 However, there is no clinical research to suggest that vaping and electronic cigarettes are effective in quitting smoking long-term; in fact, they may have higher addictive potential compared to conventional cigarettes in younger people14 and contribute to relapse and sustained dependence on nicotine products, including the electronic cigarettes and combustible cigarettes, making it difficult to quit smoking.15-17 Furthermore, national health authorities and agencies advise against the use of such products, especially those purchased on the street (bootlegger). This is due to increasing national clinical reports of serious respiratory illness known as “e-cigarette or vaping product use-associated lung injury” or EVALI and even death directly related to these products.18 The long-term effectiveness and safety of electronic cigarettes or vapes are not known, and using them is not recommended at this time.
Individual and Behavioral Counseling and Quitting Smoking
Nicotine replacement therapy and non-nicotine medication therapies clearly show effectiveness in helping people quit smoking long-term. There is also good scientific evidence that individual and behavioral counseling sessions, as a stand-alone therapy or when combined with nicotine replacement therapy or non-nicotine medication therapy, significantly improve the sustained success rates of quitting smoking.7, 19-20 The more counseling support provided can further increase rates of smoking cessation by 10 to 20%.21
Support Groups
Support groups are often available through local community centers, medical centers, hospitals, public health departments, and local chapters of the American Lung Association and American Heart Association. Someone trained in tobacco cessation counseling usually runs these groups. The support groups can be an excellent way to connect with other people who are working on quitting, gather tips and ideas about how to quit successfully and find much-needed support when trying to quit and staying quit for good.
Complementary and Alternative Medicine Approaches to Quitting
There are many complementary and alternative therapies available that may be helpful to quit smoking. Some of the more common and popular methods are acupuncture or acupressure, hypnosis, massage, and herbal preparations or medicines. These approaches have not been widely studied, and current research does not show these methods are effective in long-term success in quitting smoking. However, some have contributed to long-term quit success when combined with other evidence-based therapies, as discussed in this chapter.22-23
Technology Based and Remote Cessation Support
Web-based/Online support
There are web-based smoking cessation resources on the internet. These online resources provide support and counseling options. There is not much existing evidence that these resources are highly effective when used as the only approach to quitting smoking.24 However, using them in combination with nicotine replacement and non-nicotine therapy likely adds benefit in quitting smoking.25
American Lung Association/Freedom from Smoking
https://freedomfromsmoking.org/
U.S. Department of Health and Human Services
https://smokefree.gov/
Become An EX
https://becomeanex.org
Quitlines
There are telephone quitlines available in most states. The services they offer vary depending on the funding for that program, but they typically provide telephone counseling by trained quit coaches plus follow-up telephone calls. The counselors are trained in helping people quit smoking and can assist in making a personalized quit plan. They will provide educational resources, and many will mail nicotine replacement therapy, including the long-acting nicotine patch and either the gum or lozenge, for free. With a prescription, some can offer medications like bupropion (Zyban or Wellbutrin) and varenicline (Chantix) at a reduced cost.
The quitline specific to any state in the U.S. or any of the Canadian provinces can be located by calling the North American Quitline Consortium (NAQC) at 1-800-QUIT-NOW (U.S.) and 1-866-366-3667 (CANADA). You can also find out about local resources through your local public health department or search online using your specific state or city and “quit smoking” as keywords.
Many employers, especially large employers, have contracts with a professional quitline service that employees, and even family members of employees, can benefit from. The services and resources they provide are similar to the public quitlines. Call your Human Resources department at your job to see if they provide this benefit and cover smoking cessation medications, including over-the-counter nicotine replacement therapy.
How to Deal with Lapse and Relapse
When quitting smoking, it is common to experience a lapse in the quit attempt. A lapse is when a single or a few cigarettes are smoked. A relapse is when regular smoking is resumed and lasts longer than seven days. It often occurs when people encounter strong triggers for smoking, including stressful situations or events.5 This can also occur if treatment is disrupted or stopped too soon.
 Lapses and relapses are sometimes part of the road to success in quitting long-term.7 When a lapse or relapse occurs, people often feel bad about this disruption in the success of their quit attempt. In either case, it is possible to resume the quit attempt successfully. This can be done by returning to the approaches and methods that helped quit in the first place and reach out to your health care provider and other support systems. Avoid negative talk to yourself or others who have had a lapse or relapse, and remember to avoid triggers and focus on previous success and the goal of quitting for good.
Lapses and relapses are sometimes part of the road to success in quitting long-term.7 When a lapse or relapse occurs, people often feel bad about this disruption in the success of their quit attempt. In either case, it is possible to resume the quit attempt successfully. This can be done by returning to the approaches and methods that helped quit in the first place and reach out to your health care provider and other support systems. Avoid negative talk to yourself or others who have had a lapse or relapse, and remember to avoid triggers and focus on previous success and the goal of quitting for good.
Identifying Triggers to Smoke
When quitting smoking, it is important to address your lifestyle, rituals, and behaviors associated with and trigger smoking. Make a list of activities, people, or things that trigger the urge to have a cigarette. Be aware of these triggers and, if possible, make a plan to avoid them by restructuring daily routines and intentionally develop new rituals in your life that do not include cigarettes. It can be helpful to tell people close to you or those you frequently encounter that you are quitting smoking; this will help them support you in your efforts.
Conclusion
Quitting smoking is one of the best actions you can take to protect your health. Quitting also helps your body prepare for and optimally respond to medical treatment and enhances your ability to avoid complications and heal following surgery.26 Regardless of how long you have smoked, quitting smoking has immediate and long-term health benefits; it’s never too late to quit.5 It can be challenging to quit, but with the right tools and knowledge about the best and most effective approaches to quitting smoking, quitting is a more realistic and obtainable goal.

References
- Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults – United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013-1019.
- Lee CW, Kahende J. Factors associated with successful smoking cessation in the United States, 2000. Am J Public Health. 2007;97(8):1503-1509.
- Hughes JR, Stead, L.F., Hartmann-Boyce, J., Cahil, K., Lancaster, T. Antidepressants for smoking cessation. Cochrane Library. 2014.
- Centers for Disease Control and Prevention. Chemicals in tobacco smoke. 2014; http://www.cdc.gov/tobacco/data_statistics/sgr/2010/consumer_booklet/chemicals_smoke/. Accessed August 12, 2014.
- McEwen A. Manual of smoking cessation : a guide for counsellors and practitioners. Oxford; Malden, MA: Blackwell Pub.; 2006.
- Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Library. 2013;5:CD009329.
- S. Department of Health & Human Services. Treating Tobacco Use and Dependence: 2008 Update. Public Health Service; 2008.
- Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Library. 2018;5:Cd000146.
- Rigotti N. Pharmacotherapy for smoking cessation in adults. Up To Date. 2021.
- Burke MV, Ebbert JO, Hays JT. Treatment of tobacco dependence. Mayo Clin Proc. 2008;83(4):479-483.
- Howes S, Hartmann-Boyce, J., Livingstone-Banks, J., Hong, B., Lindson, N.et al. Antidepressants for smoking cessation. Cochrane Library. 2020.
- Leone FT, Zhang Y, Evers-Casey S, et al. Initiating Pharmacologic Treatment in Tobacco-Dependent Adults. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med. 2020;202(2):e5-e31.
- Hartmann-Boyce J, McRobbie, H., Lindson, N., Bullen, C., Begh, R., Theodoulou, A., Notely, C., Rigotti, N., Turner, T., Butler, A., Franshawe, R., Hajek, P,. Electronic cigarettes for smoking cessation. Cochrane Library. 2021.
- Jankowski M, Krzystanek M, Zejda JE, et al. E-Cigarettes are More Addictive than Traditional Cigarettes-A Study in Highly Educated Young People. Int J Environ Res Public Health. 2019;16(13).
- Hajek P, Phillips-Waller A, Przulj D, et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N Engl J Med. 2019;380(7):629-637.
- Everard CD, Silveira ML, Kimmel HL, Marshall D, Blanco C, Compton WM. Association of Electronic Nicotine Delivery System Use With Cigarette Smoking Relapse Among Former Smokers in the United States. JAMA Netw Open. 2020;3(6):e204813.
- Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. 2013;382(9905):1629-1637.
- Centers for Disease Control and Prevention. Smoking & Tobacco Use. Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products 2021; https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#cdc-recommends. Accessed June 01, 2021.
- Lancaster T, Stead, L.F. Individual behavioural counseling for smoking cessation. Cochrane Library. 2017.
- Stead L, Koilipillai, P., Fanshawe, T., Lancaster, T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Library.
- Hartmann-Boyce J, Hong, B., Livingstone-Banks, J., Wheat, H., Fanshawe, T. Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Library. 2019.
- Barnes J, McRobbie, H., Dong, C., Walker, N., Hartmann-Boyce, J. Hypnotherapy for smoking cessation. Cochrane Library.
- White A, Rampes, H., Liu, J., Stead, L., Campbell, J. Acupuncture and related interventions for smoking cessation. Cochrane Library.
- Taylor G, Dalili, M., Semwal, M., Civijak, M., Sheikh, A., Car, J. Internet‐based interventions for smoking cessation. Cochrane Library.
- Matkin W, Ordonez-Mena, J., Hartmann-Boyce, J. Telephone counseling for smoking cessation. Cochrane Library.
- Warner D, Preston, P., Subramanyam, R., Smoking or vaping: Perioperative management. Up to Date.

 Introduction
Introduction