Lung Cancer Choices© 6th Edition Menu
Chapter 1: Diagnosis and Staging of Lung Cancer
Chapter 2: Comprehensive Biomarker Testing
Chapter 3: Surgery for Lung Cancer Patients
Chapter 5: Radiation Therapy for Non-Small Cell Lung Cancer
Chapter 6: Treatment for Small Cell Lung Cancer
Chapter 7: Clinical Trials and Emerging Therapies for Lung Cancer
Chapter 9: Nutrition in the Patient with Lung Cancer
Chapter 10: Sexuality and Lung Cancer
Chapter 11: Integrative Medicine, Complementary Therapies, and Chinese Medicine in Lung Cancer
Chapter 12: Lung Cancer in People who have Never Smoked
Chapter 13: How to Quit Smoking Confidently and Successfully
Lung Cancer Question Builder - Develop your list of "Questions to Ask" your providers
Integrative Medicine, Complementary Therapies, and Chinese Medicine in Lung Cancer
Misha Ruth Cohen, OMD, LAc
Introduction
The terms “integrative medicine” and “integrative oncology” are now widely accepted as the terminology to describe complementary therapies that are used as supportive treatment as part of multidisciplinary and interdisciplinary conventional cancer care.
The National Center for Complementary and Integrative Health (NCCIH) at the National Institutes of Health (NIH) redefined integrative medicine as integrative health. Integrative health is described as medicine that “combines mainstream medical therapies and complementary and alternative medicine therapies for which there is some high-quality scientific evidence of safety and effectiveness.”
In the 2013 guidelines published in Chest on complementary therapies and integrative medicine for lung cancer, integrative oncology “refers to the study and use of complementary modalities that are not traditionally part of modern Western medical practices but can be used as adjuncts to mainstream medicine to control the symptoms associated with cancer and cancer treatment.”1
Integrative medicine and complementary therapies in lung cancer may include Chinese medicine, Western herbal therapy, relaxation and visualization techniques, prayer, exercise, nutritional supplementation, and dietary therapy. In this chapter, the primary focus will be on Chinese medicine and related therapies that may be used in conjunction with other integrative medicine and Western medicine for supporting people diagnosed with lung cancer.
Chinese Medicine
In China and many parts of the United States today, people with various types of cancer seek out Chinese medicine in addition, or as an alternative, to Western medical treatment. In lung cancer, Chinese medicine is used primarily for supportive adjunctive care in conjunction with Western treatments of surgery, chemotherapy, and radiation therapy. When intensive Western therapies are being used, Chinese medicine can relieve adverse side effects and improve the treatment outcome.
In 2007 and 2013, a multidisciplinary panel of experts in oncology and integrative medicine updated the guidelines and made recommendations on complementary therapies for use in lung cancer patients. These include acupuncture, massage therapy, mind-body modalities, nutrition, botanicals, and exercise.1-2 In the evidence-based clinical practice guidelines, the American College of Chest Physicians (ACCP) panel recommended that all patients with lung cancer be asked specifically about the use of Complementary and Alternative Medicine (CAM) and given counseling as it is important to minimize potential harm or delay in treatment. In addition, the panel concluded that mind-body modalities and massage therapy can decrease anxiety, mood disturbance, and chronic pain; acupuncture may help control pain and other side effects, and herbal products and other dietary supplements should be evaluated for side effects and potential interactions with chemotherapy and other medications.1-3
 In 2018, a review was published in the Journal of Alternative and Complementary Medicine that may provide a basis for discussion that can enhance patient-doctor dialogue regarding the use of CIM during and after treatment for lung cancer.4
In 2018, a review was published in the Journal of Alternative and Complementary Medicine that may provide a basis for discussion that can enhance patient-doctor dialogue regarding the use of CIM during and after treatment for lung cancer.4
In China, where Chinese medicine is used in conjunction with Western medicine in hospitals and clinics, men and women undergoing various treatments for cancer are offered the choice to use Chinese herbal medicine, acupuncture, Qi Gong, and exercise as adjunctive therapies to reduce side effects and increase the efficacy of the Western treatment.5 Extensive research about CAM is being done in Chinese hospitals and oncology settings in conjunction with Western research approaches and treatments.
Chinese medicine is a system of medicine that has been used for thousands of years in the treatment of health imbalances and disease. Therefore, there is a particular interest in exploring research about Chinese traditional medicine in cancer and treatment options.
The Foundations of Chinese Medicine
Traditionally, Chinese medicine has relied on the following forms of treatment to prevent or remedy disease and disorders: herbal therapy, acupuncture, acupressure/massage, dietary therapy, and exercise and meditation (often in the form of Qi Gong). These therapies are used to help the body restore balance and harmony in the mind, body, and spirit, especially when the body is attacked by a disease-causing “pernicious influence” or disrupted by internal imbalances.
There are three main areas of contrast between Western and Chinese medicine: general approach to symptoms and disease, approach to cancer, and synergy between Western and Chinese medicine.
General Approach to Symptoms and Disease
The Western medicine approach includes the design of drugs and other therapies to treat a specific disease or disorder. In Western medicine, different people who have the same diagnosis might be prescribed the same drug to treat the problem.
In contrast, a symptom such as pain may be viewed as a symptom of several possible disorders and disharmonies, affecting an individual’s mind, body, and spirit. Chinese medicine treatment focuses on identifying the underlying disharmony (diagnosis) and creating an individualized treatment suited to that diagnosis. This individualization makes double-blind controlled studies challenging to develop because each person in a study may be treated differently. However, it is sometimes possible for various types of rigorous research to be conducted.
Chinese medicine traditionally did not discuss viruses, bacteria, or cancer and did not view the immune system and disease resistance in the same way as Western medicine. Therefore, it has been difficult for Western physicians and researchers to understand that Chinese medicine treatments may attack these causes of disease.
 The goals of treatment are often different in Chinese and Western medicine. Western medicine is usually designed as an “all or nothing” proposition — either the therapy cures the disease or does not. In contrast, Chinese medicine may produce healing in the mind, body, and spirit, even in the presence of persistent disease.
The goals of treatment are often different in Chinese and Western medicine. Western medicine is usually designed as an “all or nothing” proposition — either the therapy cures the disease or does not. In contrast, Chinese medicine may produce healing in the mind, body, and spirit, even in the presence of persistent disease.
In the 21st century, Western scientific insights and Chinese treatment of the mind, body, and spirit have begun to overlap. There is no contradiction between the two systems. When clearly understood, they can strengthen and complement each other.
Approach to Cancer
Traditional Chinese medicine treatments and Western therapies approach cancer treatment from different points of view. Although most Western cancer therapies focus on killing cancer or eliminating the tumor, the primary goal of Chinese traditional medicine is to create wholeness and harmony within a person, allowing the body to heal itself. Chinese medicine strives to make the internal constitution stronger and focuses on immune functions that allow the body to fight cancer. Western medicine is just beginning to look at some of these concepts and treatments. Instead of primarily focusing on the effect of Chinese medicine treatments on tumor-eradicating abilities, it may be more beneficial to study the effect of Chinese traditional medicine on immune responses.
Chinese medicine should be evaluated on its terms and in light of its own treatment goals and objectives, not in terms of treatment goals and objectives defined by Western medicine. In Western medicine, the focus is on eradicating illness after it appears in the body. In contrast, Chinese traditional medicine has a focus on disease prevention, accomplished by creating balance and harmony in the body’s various systems.
Studies that evaluate the efficacy of a treatment to prevent disease are complicated and take many years to complete. These studies are needed to understand the efficacy of Chinese medicine fully.
Chinese medicine and other therapies that might be used as alternative therapies are most commonly used in Asia as primary therapy in treating early stages of certain types of cancer, although not as primary treatment in lung cancer. However, most Western studies are designed to evaluate the effectiveness of Chinese medicine in treating very late-stage cancers. Yet, this is frequently a stage when any treatment may be much less successful, harder to tolerate, or more difficult for patient compliance. The rationale for this research is that if it works in very late stages, then it is likely to work in earlier stages. However, in traditional Chinese medicine literature, there is little indication that the recommended Chinese medicine therapies will stop cancer in a very late-stage. Nevertheless, studies that focus on supportive treatment and palliative care in late-stage disease may be helpful. Dismissing a treatment because it is not effective in very late-stage cancer may deny scientists and practitioners the opportunity to study an effective treatment for early-stage cancer.
Synergy between Western and Chinese Medicine
The simultaneous use of traditional Chinese medicine therapies may improve Western medicine. In China, and some centers in the West, people undergoing chemotherapy, surgery, and radiation therapy treatment have the choice to use Chinese medicine therapies as adjuncts to decrease side effects and increase the efficacy of Western medical treatment.
Chinese Herbal Medicine
There are many Chinese and Western herbs used by people with cancer. A qualified, certified practitioner of herbal medicine should prescribe herbs. In some states, where practitioners are licensed to practice acupuncture or naturopathic medicine and are also qualified to practice herbal medicine, that is a big plus. Licensure, in many states, does not include herbal medicine. Therefore, national certifying bodies, such as the National Commission on the Certification of Acupuncture and Oriental Medicine, give diplomas based on professional qualifications (example – graduation from a nationally accredited college) in conjunction with passing a rigorous examination. My opinion is that licensed practitioners are required to adhere to professional standards for safety and more likely to be safe (their licenses depend on it). Licensed practitioners often use formulas that are practitioner-based, which generally have a higher safety and authenticity profile of herbal formulations. This may also be true for diplomates in states without licensure that includes herbal medicine. The patient may inquire about the professional training of the practitioner and the types of herbs used.
Chinese Herbs Used in Adjunctive Cancer Treatment
The list of herbs used in adjunctive support for cancer treatment is growing. There are individual herbs such as Astragalus (Huang Qi), American Ginseng (Xi Yang Shen), Ganoderma Mushroom (Ling Zhi, or Rei Shi), Maitake Mushroom, and Cordyceps (Dong Chong Xia Cao) that are used in cancer supportive treatment. The type of herbs used may vary with the severity of the disease, type of disease, and treatment (chemotherapy, radiation, surgery, or immunotherapy).
Some herbs may be contraindicated with some types of chemotherapy, and others may improve the effect of chemotherapy. Herbal formulas based on Astragalus may increase the effectiveness of platinum-based chemotherapy.3 Furthermore, a large treatment effect was found when adding Astragalus-based herbal treatment to standard chemotherapy regimens for non-small cell lung cancer. Specifically, the Astragalus-based herbal treatment improves survival, increases tumor response, improves performance status, or reduces chemotherapy toxicity.3
Formulas based on Ji Xue Teng (Spatholobus) are used to help support people with cancer during and after chemotherapy and radiation treatments. Support includes improving levels of fatigue, improving blood counts, and decreasing anemia and neutropenia, allowing for fewer side effects of medications, and importantly, increasing the ability of a person undergoing chemotherapy and radiation treatment to fulfill the treatment plan developed by the oncology team.
New research in 2018 of 6,939 lung cancer patients in Taiwan investigated the frequencies and patterns of Chinese herbal medicine treatment for lung cancer patients and its effect on their survival probability. The conclusion was that the use of Chinese herbal medicine as adjunctive therapy might increase survival of lung cancer patients.6
Herbal formulas based on the Chinese herb Ji Xue Teng (Spatholobus) may decrease bone marrow suppression and may enable the continuation of chemotherapy treatments at a normal schedule. In mice, an extract of Spatholobus may stimulate the proliferation of bone marrow cells and relieve the bone marrow depression caused by chemotherapy.7
Timothy Ross, DAOM has documented possible supportive Chinese herbal medicine therapies for reducing radiation damage in his presentation: “Strategies to Increase Treatment Efficacy, Reduce Harm of Ionizing Radiation, Potentiate Chemotherapy, Protect Normal Cells, Potentiate the Immune System”.8
Dr. Ross reported on an article published in 2021 “Review of the Efficacy and Mechanisms of Traditional Chinese Medicines as a Therapeutic Option for Ionizing Radiation Induced Damage in Frontiers in Pharmacology”, Zhang et al 2021 has found evidence for reducing damage from radiation in mice and cell studies by common Chinese herbs ginseng, American ginseng, astragalus, dang gui, Siberian ginseng and ginger along with a host of other herbs used by traditional Chinese herbalists. He also reported on studies of common complex herbal prescriptions such as Si Wu Tang and Bu Zhong Yi Qi Tang.
Dr. Ross stated that the mechanisms of action of Chinese herbal medicines in preventing radiation injury include:
- Reduce DNA damage
- Promote DNA repair
- Regulate cell cycle arrest
- Prevent excessive accumulation of ROS and inhibits oxidative damage
- Suppress extrinsic and intrinsic apoptotic pathways via reduction of P53, caspase, BAX/Bcl2 activation
- Regulation of inflammatory response
- Participate in the regulation of multiple abnormally activated signaling pathways.
Dr. Ross also presented a review published in 2014 by Mehta et al in Targeted Oncology “Curcumin and lung cancer—a review”. Curcumin was shown to potentiate the antitumor effect of some anti-cancer medications. Curcumin reduces side effects such as gastrointestinal effects of chemotherapies, exerts a cytotoxic effect on the NSCLC cell line, can be used as an adjunct along with standard chemotherapeutic agents, and can prevent carcinogenesis.9
Drug-Herb Interactions
The use of Chinese medicine as part of lung cancer treatment may be optimized with practitioners who use traditional methods together with modern research practices. Western practitioners, such as licensed naturopathic or integrative medical doctors, may use CAM treatments that are evidence-based. Traditional herbal and dietary methods have been used for centuries, but newer technologies of nutritional supplementation and concentrated herb extracts should be studied for safety and efficacy.
There are conflicting opinions and evidence about the use of herbs and supplements together with chemotherapy and radiation therapy, particularly among oncologists and cancer researchers who may be more focused on ensuring proper chemotherapy and radiation therapy than on the herb or supplement program. Therefore, it is important to be aware of potential adverse interactions between drugs, herbs, and some supplements, and the practitioner should consider the most up-to-date information to ensure maximum safety and efficacy.
Practitioners of Chinese and herbal medicine may provide the patient’s Western physician, oncologist, pharmacist, or other healthcare providers with information about the individualized treatment. It is important to disclose all herbs and supplements proposed for a patient’s treatment to the oncology team for review before implementing the treatment plan. This is a prudent course of action for all practitioners who work with cancer patients, especially those undergoing intensive chemotherapeutic treatments.
Chinese medicine studies that emphasize the alleviation of side effects and improving Western treatment may be the most beneficial to pursue presently, in addition to studies about cancer prevention.
Herb and Supplement Certification
Herbal formulas and nutritional supplements may be manufactured to different standards of purity and quality, such as Good Manufacturing Practices (GMP) for food or pharmaceutical products. Pharmaceutical GMP standards are stricter than food standards, and this may be important for the potency of a product. Furthermore, pharmaceutical GMP includes higher standards of testing for pesticides, toxins, bacteria, and molds, and proper identification of label ingredients. The GMP standards provide guidelines for the manufacturing site, methods of production, and quality control. Manufacturing guidelines vary from country to country. For example, Australian standards are among the strictest in the world, because Australian dietary and herbal supplements are subject to the same guidelines as pharmaceuticals, which is not the case in the United States, although there is a recent move in that direction within the United States. The guidelines require attention to manufacturing processes, including cleanliness of buildings and grounds, equipment maintenance, personnel and training, sanitation and hygiene, air and water purification, production, and documentation. It is advised that patients ask practitioners about the company that manufactures the herbs, including company location, formulas, and manufacturing standards, and defer taking herbal formulas or supplements until this information is available.
Companies can provide certificates of analysis for their products. A certificate of analysis is an authenticated document, issued by an appropriate authority that certifies the quality and purity of pharmaceuticals, animals, and plants being produced or exported. This certificate documents the formula for the ingredients, the amount of each raw material and ingredient, and the results of all the tests performed on a particular lot of the product. In some cases, albeit rare, herbs may be misidentified and added to formulas without proper authentication. Most cases of herbal toxicity are not caused by appropriate herbs given in the correct doses but are caused by the inclusion of the wrong herb or supplement in a formula. Therefore, herb identification and authenticity is an important aspect of herb manufacturing.
Acupuncture
Acupuncture is the art of inserting fine sterile metal needles into certain body or ear points to control the body’s energy flow. Acupuncture is painless and often accompanied with a sensation of heaviness, warmth, or movement of energy at the insertion point or along the energy channels. Acupuncture may relieve pain, rebalance energy, and heal symptoms. Electrostimulation also may be used with acupuncture for pain.
Western science has documented several mechanisms to explain how acupuncture works.10 Acupuncture may stimulate serotonin levels within the brain, resulting in a sense of well-being and pain relief.11 In addition, acupuncture has anti-inflammatory effects, which may help relieve symptoms and decrease inflammation. Acupuncture also may be effective in improving liver function, evidenced by improved liver function tests (transaminases).12
Acupuncture and acupressure as adjunctive cancer treatment have been studied for postoperative nausea and vomiting, chemotherapy-related nausea and vomiting, and pain relief.11An observational study of acupuncture in lung cancer showed significant improvements in pain, appetite, nausea, nervousness, and well-being.13 Acupressure is a type of massage or touching therapy that uses the principles and theory of acupuncture and Chinese medicine. In acupressure, the same points as acupuncture are used on the body, but these are stimulated with a finger or other pressure instead of inserting needles.
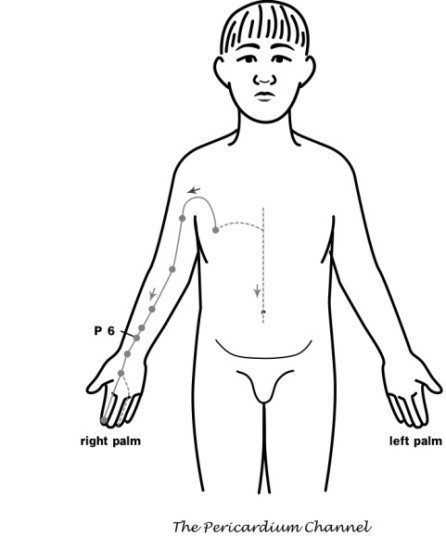
Several studies have evaluated acupuncture point Pericardium 6 (P6) for both acupuncture and acupressure in nausea and vomiting resulting from chemotherapy and surgery. When electroacupuncture was used for the prevention of postoperative nausea and vomiting, electrostimulation of acupuncture points or ondansetron was more effective than a placebo, with a greater degree of patient satisfaction. However, electrostimulation of acupuncture points was more effective than ondansetron in controlling nausea. Stimulation of the acupuncture point P6 also may relieve pain, and electroacupuncture had better pain relief in the recovery room than either ondansetron or placebo.14 The 2013 ACCP guidelines recommend acupuncture and related techniques (with the caveat that the evidence is somewhat weak) in patients having nausea and vomiting from either chemotherapy or radiation therapy, as well as an adjunct treatment option as in patients with cancer related pain and peripheral neuropathy with inadequate control of symptoms.15
Acupressure and Massage
Many forms of massage and bodywork can be used by people diagnosed with lung cancer including acupressure, Tui Na (Qi Gong), shiatsu, Thai massage, deep tissue massage, and long stroke massage (including Esalen and Swedish). Several studies show improvement of symptoms in people with cancer who receive massage. In a study of 1290 people with cancer who received a massage, symptom scores were decreased by 50%.16
Several studies in the use of the acupuncture point Pericardium 6 (P6) in women with breast cancer showed that nausea and vomiting from chemotherapy might be decreased when used in conjunction with conventional drug treatments. Furthermore, a large clinical trial performed in several cancer centers concluded that acupressure was helpful at decreasing the amount and intensity of chemotherapy-induced nausea and vomiting in women with breast cancer.14
People with cancer are best treated by specially trained practitioners trained in oncology massage, who know which areas to avoid and which kind of bodywork is appropriate. Swollen areas, fractures, skin infections, or severe hematomas should not be massaged. A Western healthcare practitioner should check lumps and areas of swelling before massaging. It is best to seek medical advice before having therapeutic bodywork if the patient has phlebitis, thrombosis, varicose veins, severe acute back pain, or fever. Consultation is especially important in immunocompromised individuals, including people having chemotherapy, patients with HIV infection, and others with low immunity.
 The Society for Oncology Massage states:
The Society for Oncology Massage states:
“Oncology massage does not try to “fix” anything and, unlike many massage modalities, is not a series of techniques or applied protocols. Rather, it is the ability of the therapist to recognize and safely work within clinically established guidelines, considering the patient’s unique circumstance… Oncology massage education for massage therapists is important for clinical safety and therapeutic benefit. Adaptations to massage therapy techniques may be indicated both during treatment and for the rest of a person’s life after treatment.”17
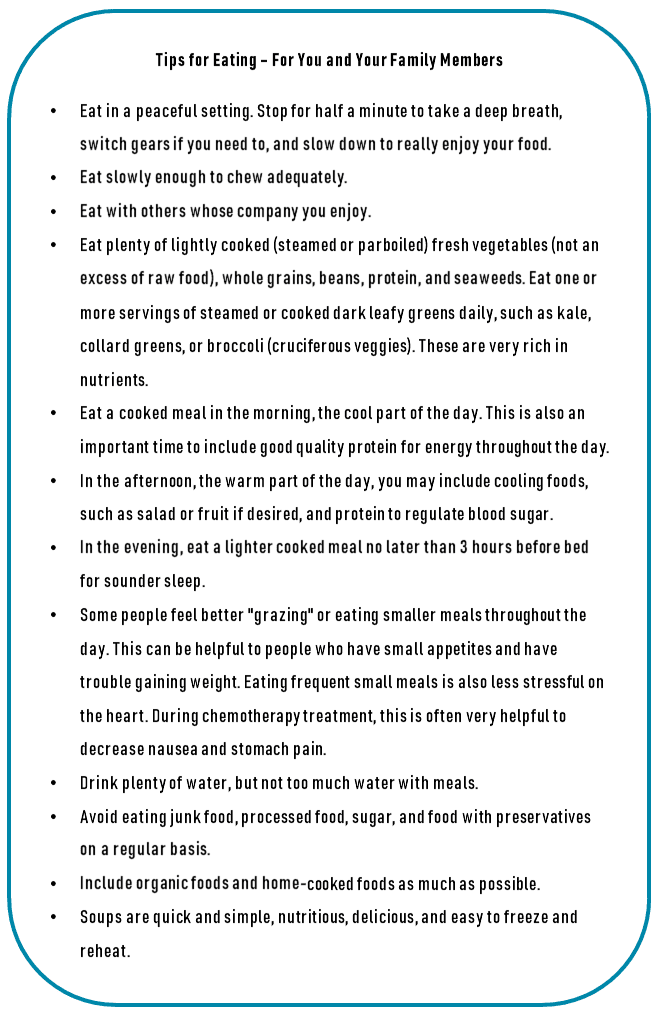
Food Therapy
 Dietary therapy is an important part of Chinese medicine and complementary and alternative medicine. In Chinese medicine, food therapy and diet are the first treatments given to people who are trying to stay well and remain in balance or who are experiencing illness. In Chinese thought, the digestion must be kept healthy or a person can easily become ill. Food intake is very important to healthy digestion and assimilation of food. Therefore, anything that disrupts the function of the organs of digestion is damaging to the body’s energy.
Dietary therapy is an important part of Chinese medicine and complementary and alternative medicine. In Chinese medicine, food therapy and diet are the first treatments given to people who are trying to stay well and remain in balance or who are experiencing illness. In Chinese thought, the digestion must be kept healthy or a person can easily become ill. Food intake is very important to healthy digestion and assimilation of food. Therefore, anything that disrupts the function of the organs of digestion is damaging to the body’s energy.
Some of the concepts of Chinese medicine most important for digestion include eating at regular times and eating cooked foods. Chinese medicine theory considers that energy is required to warm the stomach to digest foods, and cold and raw foods may be harmful to the digestive energy and should be eaten sparingly; this is especially important for people who have been sick and have had stomach pain and nausea often due to cancer treatment. (The issue of raw or cooked food is controversial, and raw food advocates argue that cooking may destroy enzymes in food important to digestion.) Furthermore, Chinese medicine advocates eating foods that are in season and grown as close to home as possible, because these foods are fresher and have more food energy and more Qi. Herbs can be added to foods to increase food vitality, especially for specific health conditions.
While there are different approaches to food therapy currently used in the West, traditional methods that have been used in Chinese medicine are still used today. For example, we now know that the type and amount of carbohydrates in the diet is very important in maintaining good health. It is especially important to focus on the glycemic index of carbohydrates to improve insulin sensitivity. In our clinic, we combine traditional methods with modern understandings of using food to promote health, including reducing cancer risk. This is discussed more fully in The New Chinese Medicine Handbook.18
 Taking this into account, traditionally, rice is the basic food used for healing in Chinese medicine, although other grains may be used, including quinoa, barley, rye, and buckwheat. Some people will need to avoid grains with gluten, such as barley and rye, due to gluten sensitivity. Congee is a special grain porridge that is considered traditionally to be a very therapeutic food and used during chronic weakness diseases and convalescence from illnesses. When people diagnosed with lung cancer are being treated with chemotherapy, recovering from surgery, or having other debilitating treatments, congee is a good and easy option for nutrition and recovery. There are many varieties of congee suitable for different conditions and symptoms, and a Chinese medicine practitioner can provide recipes specific to the patient’s situation.
Taking this into account, traditionally, rice is the basic food used for healing in Chinese medicine, although other grains may be used, including quinoa, barley, rye, and buckwheat. Some people will need to avoid grains with gluten, such as barley and rye, due to gluten sensitivity. Congee is a special grain porridge that is considered traditionally to be a very therapeutic food and used during chronic weakness diseases and convalescence from illnesses. When people diagnosed with lung cancer are being treated with chemotherapy, recovering from surgery, or having other debilitating treatments, congee is a good and easy option for nutrition and recovery. There are many varieties of congee suitable for different conditions and symptoms, and a Chinese medicine practitioner can provide recipes specific to the patient’s situation.
The basic method of making congee is to cook one cup of rice (or other grains) in seven to nine cups of filtered water for six to eight hours. Cooking can be done overnight, and it is ideal to use a slow cooker such as a crockpot or any cooking pot. Herbs with or without meat or vegetables are added as directed by the Chinese medicine practitioner for the patient’s specific condition. In our clinic, we highly recommend that the glycemic index and load of the grains be offset by using a substantial amount of protein and vegetables to have the best healing properties.
Traditional Chinese families serve congee to the whole family weekly with herbs such as Ginseng, Dong Quai, Codonopsis, Red Dates, Ginger, and Astragalus. Astragalus is good in immune tonic congee. Soups are highly recommended in Chinese food therapy. Chicken soup is considered very healing by the Chinese, and many soups that are tonics are based on chicken broth. Congees may also use chicken broth as a base with specific herbs for the patient’s condition.
Qi Gong: Exercise and Meditation
The Benefits of Exercise in Lung Cancer
Chronic or life-threatening illness can make a person feel as if the body is beyond his or her control. Exercise and meditation can take control over quality of life and the vitality of the mind, body, and spirit. Exercise can help decrease stress and depression, strengthen the cardiovascular system, improve appetite, maintain muscle mass, improve and maintain digestion, and avoid constipation or diarrhea associated with the medication.
Moderate exercise is recommended, starting with 20-minute periods, three times weekly. The benefits of exercising are extensive, and regular exercise is advised. However, stamina and tolerance for stress may ebb and flow during the course of disease and treatment. Therefore, break periods may be required, and exercise programs may be resumed when the patient has more energy and endurance.
In the general population, regular exercise that oxygenates the blood and tones the muscles helps people live longer, look younger, and think more clearly. Exercise also has emotional and spiritual benefits. In general, people with a normal stress response should get as much exercise as possible. However, patients who have lung cancer must evaluate the risks of exacerbating symptoms because of overexertion, and Qi Gong may be helpful in this situation.
Benefits of Qi Gong Exercise
Qi Gong is the traditional Chinese discipline that focuses on breathing and movement of Qi (“life force”) to increase physical harmony and strength and establish spiritual and emotional peace.19 There are numerous different schools of practice, some very vigorous (including martial arts) and others extremely gentle. Careful, relaxed breathing is the foundation of most Qi Gong movements.
The energy-conserving, Qi-channeling practice of Qi Gong is designed to keep a person healthy and fit without causing stress and exhaustion. Furthermore, patients who have excessive fatigue, shortness of breath, fluid retention, or neuropathy may be required to avoid strenuous exercise; in these situations, Qi Gong meditation and breathing exercises can become the primary way to obtain exercise.
The Chinese practice of Qi Gong may improve outcomes for people with cancer, including improved immune responses and decreased symptoms associated with cancer treatment. However, most studies are small, and the evidence is varied. Qi Gong therapy may have an inhibitory effect on cancer growth, both in vitro and in vivo, but repeat studies are unavailable for confirmation.19 Furthermore, Qi Gong in cancer patients may improve quality of life and mood status and decrease inflammatory markers and side effects of cancer treatment.5 A systematic review published in 2018 in The Journal of Cancer Survivorship concluded that Tai Chi and Qigong show promise in addressing cancer-related symptoms and quality of life in a variety of cancer survivors.20
Exercise: The Circle of Qi
This exercise was designed by Qi Gong master Larry Wong of San Francisco to circulate Qi throughout the body, replenish depleted Qi, and calm the Shen (spirit).
Sit on the floor cross-legged style or in a lotus position. If that is uncomfortable, you may stand up or lie down during these breathing routines.
Inhale to a count of four to eight, depending on comfort. There are two breathing techniques you can use, Buddha’s Breath, and Taoist’s Breath.
For Buddha’s Breath, inhale, extending your belly as you fill it up with air from the bottom of your lungs upward; exhale by pushing the air out from the bottom of your lungs first, contracting the lower rib cage and abdominal muscles, and then the upper torso.
For Taoist’s Breath, inhale, contracting your abdomen; exhale, letting your abdomen relax outward. You may practice these breathing techniques on alternate days.
As you inhale, imagine the air and your Qi flowing evenly along the pathways of the channels.
Become aware of the air as it enters through your nostrils and moves down the center of your chest to a spot on your abdomen about 1 to 2 inches below the navel. This is the area of the body called the dan.
Now breathe out slowly and evenly, releasing the breath from the abdomen, up through the lungs, and out your slightly open mouth.
As you exhale, imagine that the Qi that was at the dan is moving down through your pelvis, through your crotch, and up your tailbone to your lower back.
Keep exhaling in a slow, steady, smooth stream that passes gently over your lips.
As you inhale again, follow the Qi as it moves up along your back to your shoulders.
Exhale and move the Qi up to the back of the head, over the top of your head, down your forehead, and returning to the nose.
At first, it may be difficult to follow the flow of Qi through its cycle. Be patient and keep your breathing calm and your mind relaxed while focusing on your inhaling and exhaling.
Conclusion
In conclusion, people diagnosed with lung cancer and other cancers has a wide range of integrative and complementary modalities to choose from, including a wide breadth of Chinese traditional medicine practices. These can often be used as adjunctive therapies to support Western conventional treatments. Side effects frequently can be ameliorated using various forms of integrative and Chinese medicine. It is best to seek out qualified – licensed when necessary – practitioners and teachers who have knowledge of cancer support in your quest to use these practices. It is important to discuss and confirm any therapies you might be considering with your Western conventional treatment team.
References
- Deng GE, Rausch SM, Jones LW et al. Complementary therapies and integrative medicine in lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines (3rd edition). 2013 May;143(5 Suppl):e420S-36S. doi: 10.1378/chest.12-2364.
- Cassileth BR, Deng GE, Gomez JE et al. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(3 Suppl):340S-354S.
- McCulloch M, See C, Shu XJ et al. Astragalus-based Chinese herbs and platinum-based chemotherapy for advanced non-small-cell lung cancer: meta-analysis of randomized trials. J Clin Oncol. 2006;24(3):419-30.
- Frenkel M, Slater R, Sapire K, Sierpina V. Complementary and Integrative Medicine in Lung Cancer: Questions and Challenges. J Altern Complement Med. 2018 Sep/Oct;24(9-10):862-871. doi: 10.1089/acm.2018.0175. Review. PMID: 30247955
- Oh B, Butow P, Mullan B, et al. Impact of medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol. 2010;21(3):608-14.
- Li TM, Yu YH, Tsai FJ, Cheng CF, Wu YC, Ho TJ, Liu X, Tsang H, Lin TH, Liao CC, Huang SM, Li JP, Lin JC, Lin CC, Liang WM, Lin YJ. Characteristics of Chinese herbal medicine usage and its effect on survival of lung cancer patients in Taiwan, J Ethnopharmacol. 2018 Mar 1;213:92-100. doi: 10.1016/j.jep.2017.10.031. Epub 2017 Oct 31. PMID: 29100936
- Fu Q , Luo X-q, Tang Y, et al. Study on Antitumor Activity in Vivo and Effect on Hematopoiesis of Extract of Spatholobus suberctus Dunn. Chinese Journal of Information on Traditional Chinese Medicine http://en.cnki.com.cn/Article_en/CJFDTOTAL-XXYY200812016.htm
- Online Webinar and Training, Personal Communications
- Mehta, H.J., Patel, V. & Sadikot, R.T. Curcumin and lung cancer – a review. Targ Oncol 9, 295-310 (2014) https://doi.org/10.1007/s11523-014-0321-1
- Shen J. Research on the neurophysiological mechanisms of acupuncture: review of selected studies and methodological issues. J Altern Complement Med. 2001;7 (Suppl 1):S121-7.
- Sugai GC, Freire Ade O, Tabosa A, et al. Serotonin involvement in the electroacupuncture- and moxibustion-induced gastric emptying in rats. Physiol Behav. 2004;82(5):855-61.
- Zijlstra FJ, van den Berg-de Lange I, Huygen FJ, et al. Anti-inflammatory actions of acupuncture. Mediators Inflamm. 2003;12(2):59-69.
- Kasymjanova G, Grossman M, Tran T, et al. The potential role for acupuncture in treating symptoms in patients with lung cancer: an observational longitudinal study. Current Oncology. 2013;20(3):152-157. doi:10.3747/co.20.1312.
- Gan TJ, Jiao KR, Zenn M, et al. A randomized controlled comparison of electro-acupoint stimulation or ondansetron versus placebo for the prevention of postoperative nausea and vomiting. Anesth Analg. 2004;99(4):1070-5.
- Dibble SL, Luce J, Cooper BA, et al. Acupressure for chemotherapy-induced nausea and vomiting: a randomized clinical trial. Oncol Nurs Forum. 2007;34(4):813-20.
- Cassileth BR, Vickers AJ. Massage therapy for symptom control: outcome study at a major cancer center. J Pain Symptom Manage. 2004;28(3):244-9.
- Society for Oncology Massage. http://www.s4om.moonfruit.org/#/health-care-professionals/4558534846
- Cohen, MR, The New Chinese Medicine Handbook: An Innovative Guide to Integrating Eastern Wisdom with Western Practice for Modern Healing. Fair Winds Press (MA).
- Chen K, Yeung R. Exploratory studies of Qigong therapy for cancer in China. Integr Cancer Ther. 2002;1(4):345-70.
- Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, Song R Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018 Apr;12(2):256-267. doi: 10.1007/s11764-017-0665-5. Epub 2017 Dec 8. PMID: 29222705